
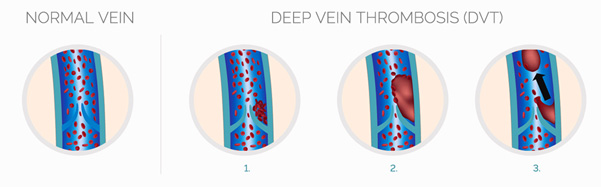
Clotting that occurs in the deep venous systems of the body are called Deep Vein Thrombosis (DVT). This occurs most commonly in the legs but can also occur in the veins of the pelvis. Other sites where clotting in the veins can occur are in the abdomen – portal vein or mesenteric vein thrombosis, in the neck and in the brain (cerebral venous thrombosis).
The veins in the legs (where DVT happens most commonly) have valves, that prevent back flow of blood into the calf and legs. These valves have cusps where stagnation of flow can happen during periods of rest and inactivity. Thrombosis most commonly happens in these valve cusps. There is a continuous mechanism of clot (thrombus) formation and dissolution that keeps on happening in the body. There are various chemicals that are involved in both these processes throughout our lifetime that keep this process of clot formation and dissolution in balance.
For example, if a clot happens in a vein valve cusp, then the body’s clot dissolution mechanism will also keep working to make sure the clot does not progress and is dissolved there itself. On the other hand, if an injury happens and it leads to bleeding, if the clotting mechanism does not activate itself, we can die of bleeding itself.
Sometimes these protective mechanisms are overwhelmed, and can result in problems of bleeding and clotting.
The most common site for the development of clots / thrombosis is in the deep veins of the legs (large veins located deep within the muscles of the leg). The reasons for development of the clots in this region are mainly prolonged bed rest, muscle injury etc. Along with immobilization, this leads to injury to the vein wall and thickening of the blood. This leads to formation of the clot in the deep venous system.
The various causes for development of VTE are:
Leg long bone fractures, major orthopedic surgeries like total hip arthroplasty, total knee arthroplasty (TKR), spine surgeries, bed rest following plaster cast application for any fractures in legs/ pelvis etc.;
after stroke, paraplegia, critically ill patients in ICU, sepsis, COVID 19 virus etc.;
Prior history of Deep Vein Thrombosis;
Major surgeries involving the abdomen, especially cancer surgeries;
Active cancer, cancer chemotherapy – drugs and indwelling catheters;
Cardiac conditions like congestive cardiac failure;
Chronic smokers, varicose veins etc.;
Prolonged travel in cramped spaces (Economy Class Syndrome), dehydration, extreme cold;
Intravenous injections given in the leg veins, indwelling catheters;
(this list is not complete and reasons other than those mentioned above can also be a cause of DVT/ PE)
The most common presenting features of VTE are pain and swelling in the involved limb. At times one may be more severe compared to the other. Very rarely, is pain absent.
Clots forming in the deep veins of the legs and pelvis can cause serious problems both in the short and long term. In the short term, the most dangerous complication is Pulmonary embolism. This occurs when a portion or whole of the clot breaks away from the clot in the leg and goes to the lungs. This leads to a sudden reduction of blood going from the heart to the lungs for oxygenation. This causes shortness of breath, falling blood pressures, rising heart rates, increased rate of breathing which can happen in varying combinations and severity. occasionally, it can be fatal. Fortunately, majority of the Pulmonary Embolism that occurs is not significant. The risk factors for development of PE are the same as that for development of DVT. Patients with a prior history of DVT who develop recurrent clots are at potentially higher risk of developing PE.
Not every individual is at risk of developing venous thrombosis. However, there are a few risk factors whose identification in time can prevent VTE from happening. There are various scoring systems (Wells, Rogers, Caprini etc.), that are used in ICU and hospitals that can help to identify which patient is at a higher than usual risk for developing VTE and can take appropriate counter-measures to prevent VTE from happening (no method is fool proof and 100% successful).
Ask your treating physician/ surgeon about the risk of VTE and the measures that will be taken for its prevention.
The simplest and fastest method to diagnose DVT is with Ultrasound (venous Duplex).
DVT can cause life threatening complications in the acute stage and lifestyle threatening complications in the late stages. The life threatening complication is Pulmonary Embolism, whereas the lifestyle threatening complication is Post Thrombotic Syndrome.
Medical management: Acute clots / deep vein thrombosis in the legs can be managed effectively by medications. Occasionally it can be managed without admission to a hospital setup. Hospitalisation is required in patients with extensive DVT with significant pain and swelling. Treatment is with blood thinners (anticoagulants – heparin, Enoxaparin, Fragmin, Fondaparinux). Oral anticoagulation can be with either Acitrom/ Warfarin or one of the newer anticoagulant drugs.
Treatment with Acitrom/ warfarin requires regular monitoring of its levels with PT/INR evaluation and dosage of the medication is adjusted to maintain the INR between 2-3. Green leafy vegetables are to be avoided during the treatment with Acitrom/ Warfarin.
Of late, newer medications are available that do not require any regular blood tests and offer the option of fixed dose therapy. The risk of bleeding with these medications is actually lower than Acitrom/ warfarin. Dietary restrictions like avoidance of green leafy vegetables are not required for these medications.
Along with medications, graduated compression garments are an absolute must, started along with the medications. They help in reduction of swelling and pain. These compression garments are to be changed every 3-4 months or as directed by your physician.
Endovascular management: Clots extending into the abdomen have a high risk of leading to Post Thrombotic Syndrome and thus require aggressive management. Occasionally, it may be necessary to dissolve the clots with thrombolytic drugs (Urokinase, Actilyse etc) so that normal blood flow can be established at the earliest. This is done in the hybrid lab with a special drug delivery catheter placed in the thrombus and the drug delivered directly to the clot. This method is called Catheter Directed Thrombolysis (CDT). It has the fastest clot dissolution rates and the highest chances of clot dissolution compared to systemic administration of thrombolytic agents. These clots can be extracted with the help of special devices and suction pumps which can further reduce the dose of the thrombolytic agent. This combination therapy (use of thrombolytic drugs and suction/ maceration of clot) is called Pharmaco-Mechanical Thrombolysis and is now considered the gold standard for treatment of this problem. Repeat visits to the hybrid lab with serial angiograms are performed during pharmacomechanical thrombolysis to note the extent of dissolution of clots. This can reveal disease occurring in the iliac veins and the IVC for which treatment can be given at the same time in the form of angioplasty and stenting. This is performed with the help of special venous stents which are of large diameters and lengths (a venous stent is often 12-20mm in diameter and 60 to 160mm in length; compared to coronary stents 2-4mm in diameter and max 48mm length). Patients are observed in the ICU while this procedure is being done. Once thrombolytic therapy is finished, injectable + oral anticoagulation therapy is started.
The average duration for treatment of DVT ranges from 3 to 6 months. The decision regarding stoppage of treatment is by evaluating the D dimer levels and venous duplex examination. However there are clinical situations wherein your clinician may decide to continue treatment for a much longer period of time. This is most commonly seen in patients with cerebral venous thrombosis, portal / mesenteric venous thrombosis, recurrent pulmonary embolism, recurrent DVT, or in patients with inherent clotting disorders detected in their blood.
Yes. Unfortunately so. Whenever a second or subsequent episode of DVT happens, the cause for the first episode also has to be relooked into. If the DVT occurs in the same limb, it is necessary to note the extent of clot dissolution from the previous duplex scans. Partially dissolved clots of <40% of the lumen are at a higher risk of developing rethrombosis.
Other causes like hypercoaguable states, underlying malignancy etc have to be evaluated.
There is a higher than normal risk of PTE if the VTE event occurs in the same limb.
In event of recurrence of DVT, treatment is often continued for a much longer period, sometimes lifelong.
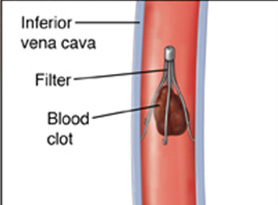
Occasionally, these anticoagulants cannot be given to a patient. These situations include recent major surgery, recent surgery on the brain/ spine, active bleeding, patients with polytrauma, low platelet counts etc. these situations have a higher than usual risk of bleeding, which can be dangerous. These are high risk situations in whom development of DVT is common. There is a higher than usual risk of clots breaking away in this patient population and migrating to the lungs causing Pulmonary Embolism.
Fatality from pulmonary embolism can be prevented by placement of IVC filters. These filters are placed in the veins in the abdomen in a nonsurgical manner. They prevent major clots from migrating to the lungs which can be potentially life threatening.
IVC filters are of two types, retrievable and permanent. IVC filters are placed to prevent pulmonary embolism till the patient can be started on anticoagulants. Hence, in the vast majority of the patients, they are temporary (just like the umbrella is kept open only till it is raining, and folded back when the rain stops). Temporary filters come with a hook at their top end so that they can be extracted easily. This is done when the contraindication to anticoagulation is no longer present and has been resolved. Filters by themselves can promote clotting when left inside for longer than necessary. Majority of the IVC filters should be removed within 15 to 45 days. Occasionally they can be kept longer necessary while the patient is on anticoagulation. The longer the filter stays inside, the harder it is to retrieve!

Secondary varicose veins are the most common problem that can be seen in the long term. Treatment of DVT in the acute phase leads to dissolution of the clots in majority of the situations provided medications are given in therapeutic doses and stockings are worn regularly. Occasionally the veins can shrink, cause webs due to the inflammation caused by the clots. This shrinking of the veins can happen in any venous segment. Shrinkage occurring in the IVC, iliac veins and common femoral vein leads to difficulty in walking, swelling, pain, ulcers that do not heal despite long term dressings, blackish discoloration of the skin around the ankle with hardening of the skin in this area.
Treatment options for shrinkage of IVC, iliac veins and common femoral veins include angioplasty and stenting, and occasionally hybrid surgical interventions are performed combining both endovascular treatment for the Iliac vein – IVC segment and open surgery for the groin webs. Regular follow-up with long term anticoagulation is necessary along with routine use of graduated compression stockings.
